Neural mechanisms and recovery of language production deficits in aphasia
This longitudinal, multimodal neuroimaging study investigates the contributions of numerous gray and white matter structures to the recovery of language production skills in aphasia during the first year post-stroke and beyond.
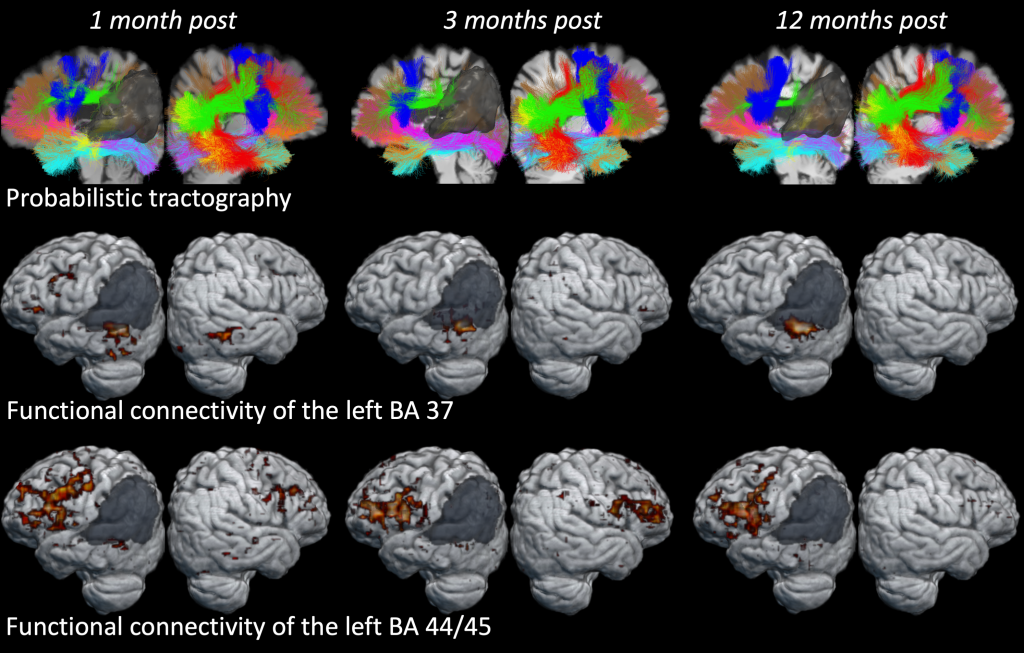
Most individuals with aphasia have difficulty producing words and sentences, which impairs their ability to communicate naturally. While some people with language production deficits recover well during the first year after injury, others will not, and this discrepancy in outcomes is largely unpredictable. The proposed project will be the first comprehensive longitudinal multimodal neuroimaging study to examine plasticity within gray matter regions and white matter tracts and their contribution to recovery of different linguistic levels involved in language production over the course of one full year and beyond. The first main objective of the study is to determine which damaged cortical regions and white matter pathways impede recovery of language production throughout the first year. The second main objective is to measure neuronal changes in gray matter morphometry and white matter integrity that accompany observed behavioral improvement.
The general outline of the study is the following. Individuals with aphasia will be tested at 1-, 3- and 12-months post stroke on various measures of language production at the word, sentence and discourse levels to establish baseline measures of performance and monitor changes across the different stages of recovery. At the same three time points, participants will undergo structural MRI and high angular resolution diffusion imaging (HARDI) to determine lesion site, white matter integrity, and changes in grey and white matter over time. The rationale for choosing these particular time points is as follows: At 1-month post onset, we will be able to assess patients in the very early stages of their aphasia, while avoiding medical issues in the most acute stage that interfere with testing and scanning, permitting a more reliable measure of initial symptoms. At 3-months post onset, significant changes will have occurred during this critical period and can be captured with our measures. At 12-months, we will be able to capture patients’ full potential for recovery, since many patients, particularly those with white matter strokes, require this amount of time to demonstrate behavioral changes.
Evaluating different time periods during the first year post-stroke will enable us to determine damage to which grey and white matter structures can predict certain patterns of recovery, and which neural changes accompany different trajectories of recovery from language production deficits. To accomplish this we will utilize several state-of-the-art neuroimaging techniques in combination with detailed language testing of different linguistic levels. First, Voxel-based Lesion Symptom Mapping (VLSM) analyses will show whether there are brain structures that, when damaged, affect the amount of recovery in language abilities in general, overall production, at the word-level, sentence-level, or discourse level, for two different periods of recovery (from 1-month to 3-months and from 1-month to 12-months). Second, we will explore the relationship between changes in language outcome measures and DTI measurements from relevant white matter pathways acquired at 1-month post onset. Finally, using multiple regression analyses we will investigate the contribution of changes in cortical morphometry (cortical thickness, local area, and myelination measures) and white matter integrity (diffusivity measures, tract characteristics) to changes in language abilities across the first year post-stroke. Evaluating different time periods during the first year post-stroke will enable us to tease out neural indices predicting, impeding, and supporting language recovery at different stages. Information resulting from this study will provide clinicians with the information they need to give people with aphasia the most accurate diagnosis, prognosis, and effective treatment to date.
As a part of this study, we are also seeking to recruit individuals with chronic aphasia due to a stroke that happened at least one year ago. We will be testing them with a similar behavioral protocol and conducting an identical MRI scan to the main group with acute aphasia. These individuals will be tested twice, one year apart. This data will help us understand how recovery in the first year is different from continued recovery at the more chronic stages.
This study is supported by NIH/NIDCD grant R01 DC016345 to Dr. Nina F. Dronkers and Dr. Maria V. Ivanova.
T.I.M.E. Project
Temporal Impairment in Mapping Events: Linguistic and Non-Linguistic Time in Aphasia

Locating events on a timeline allows us to keep track of the past, live the present and plan the future. Some individuals can lose this fundamental aspect of human existence: people with aphasia. Aphasia is a language disorder typically caused by a stroke or a head injury that affects the ability to read, write and speak coherently. The source of the time impairment in aphasia is still unknown. Previous accounts focused on the linguistic aspect of this deficit, but data coming from clinical case reports and experimental studies suggest that this impairment may not be exclusively linguistic. The main aim of this project is to carry out a systematic investigation of time processing in aphasic patients across different domains and, for the first time, through the use of structural magnetic resonance imaging. Three questions will be addressed: which aspects of time processing are impaired in aphasic patients? Is this impairment language-specific? What is the neurobiological basis of time processing? Behavioral (neurolinguistics/cognitive science) paradigms testing different aspects of non-/linguistic time processing will be combined with a voxel-based lesion-symptom mapping (VLSM) analysis and diffusion magnetic resonance imaging (dMRI). This proposal will provide answers to long-standing questions concerning the nature of time impairment in people with aphasia and the neural underpinnings of time processing. This work will also lay the foundations for the development of new clinical tools for aphasic patients suffering time impairment.
This grant is supported by the European Union’s Horizon 2020 research and innovation programme under the Marie Sklodowska-Curie grant agreement No 101028370 (PI Nicoletta Biondo).
CYCLE Project
Lesion analysis of the brain areas involved in language comprehension
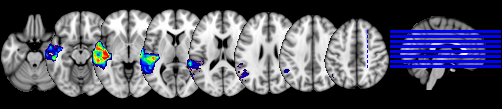
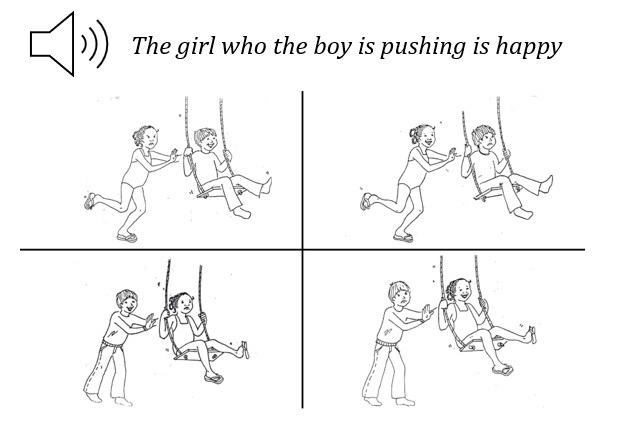
Whether syntactic comprehension, i.e., the ability to assign a hierarchical structure to a sentence in order to successfully interpret its meaning, relies mostly on frontal regions, e.g., posterior Inferior Frontal Gyrus (pIFG), or on temporal regions, e.g., posterior Middle Temporal Gyrus (pMTG), is still debated. Lesion-symptom mapping (LSM) analyses can actively inform this debate by identifying regions that are critical for specific linguistic operations. In this project, we wish to contribute to this debate by analyzing the performance of more than 100 individuals with post-stroke aphasia who were asked to perform the Curtiss–Yamada Comprehensive Language Evaluation – Receptive (CYCLE-R) test. The CYCLE-R was built to test the comprehension of sentences with different levels of syntactic complexity (from simple declarative clauses to more complex embedded relative clauses) through a sentence-picture matching paradigm. LSM analyses with both univariate and multivariate methods will be implemented to detect areas associated with the processing of sentences with different syntactic complexity.
Singing in the Brain Project
Neural Mechanisms of Song v. Speech Production: Insights from Aphasia and Intracranial Recording

Despite extensive exploration into the neural mechanisms of language, there is no conclusive explanation for why language expression through song is spared relative to speech in certain individuals with aphasia. To investigate this phenomenon, this project takes an innovative approach in examining how the brain expresses language through song versus speech. We will explore behavioral patterns and the structural and functional neuroanatomy of singing, merging evidence from two distinct patient cohorts and two different methodologies: individuals with post-stroke aphasia, and neurosurgical patients with implanted electrodes. The novel combination of behavioral and lesion analysis in people with aphasia and intracranial electroencephalography (iEEG) in neurosurgical patients will provide unique insights into the behavioral and neural mechanisms of singing.
Publications supported by the NIH Aphasia Recovery grant RO1 DC016345
Journal Articles (All published journal articles are public access compliant)
2017
- Dronkers, N. F., Ivanova, M. V., & Baldo, J. V. (2017). What do language disorders reveal about brain–language relationships? From classic models to network approaches. Journal of the international neuropsychological society, 23(9-10), 741-754. doi: 10.1017/S1355617717001126. PMCID: PMC6606454.
2018
- Paulraj, S. R., Schendel, K., Curran, B., Dronkers, N. F., & Baldo, J. V. (2018). Role of the left hemisphere in visuospatial working memory. Journal of neurolinguistics, 48, 133–141. doi: 10.1016/j.jneuroling.2018.04.006. PMCID: PMC6656388.
- Baldo, J. V., Kacinik, N., Ludy, C., Paulraj, S., Moncrief, A., Piai, V., Curran, B., Turken, A., Herron, T., & Dronkers, N. F. (2018). Voxel-based lesion analysis of brain regions underlying reading and writing. Neuropsychologia, 115, 51–59. doi: 10.1016/j.neuropsychologia.2018.03.021. PMCID: PMC6648682.
- Ivanova, M. V., Dragoy, O., Kuptsova, S. V., Yu Akinina, S., Petrushevskii, A. G., Fedina, O. N., Turken, A., Shklovsky, V. M., & Dronkers, N. F. (2018). Neural mechanisms of two different verbal working memory tasks: A VLSM study. Neuropsychologia, 115, 25–41. doi: 10.1016/j.neuropsychologia.2018.03.003. PMCID: PMC6658104.
2019
- Akinina, Y., Dragoy, O., Ivanova, M. V., Iskra, E. V., Soloukhina, O. A., Petryshevsky, A. G., Fedinа, O. N., Turken, A. U., Shklovsky, V. M., & Dronkers, N. F. (2019). Grey and white matter substrates of action naming. Neuropsychologia, 131, 249–265. doi: 10.1016/j.neuropsychologia.2019.05.015. PMCID: PMC6650369.
- De Witte, E., Piai, V., Kurteff, G., Cai, R., Mariën, P., Dronkers, N., Chang, E., & Berger, M. (2019). A valid alternative for in-person language assessments in brain tumor patients: feasibility and validity measures of the new TeleLanguage test. Neuro-oncology practice, 6(2), 93–102. doi: 10.1093/nop/npy020. PMCID: PMC6656337.
- Battistella, G., Henry, M., Gesierich, B., Wilson, S. M., Borghesani, V., Shwe, W., Miller, Z., Deleon, J., Miller, B. L., Jovicich, J., Papinutto, N., Dronkers, N. F., Seeley, W. W., Mandelli, M. L., & Gorno-Tempini, M. L. (2019). Differential intrinsic functional connectivity changes in semantic variant primary progressive aphasia. NeuroImage: Clinical, 22, 101797. doi: 10.1016/j.nicl.2019.101797. PMCID: PMC6465769.
- Lukic, S., Mandelli, M. L., Welch, A., Jordan, K., Shwe, W., Neuhaus, J., Miller, Z., Hubbard, H. I., Henry, M., Miller, B. L., Dronkers, N. F., & Gorno-Tempini, M. L. (2019). Neurocognitive basis of repetition deficits in primary progressive aphasia. Brain and language, 194, 35–45. doi: 10.1016/j.bandl.2019.04.003. PMCID: PMC6669076.
2020
- Battistella, G., Borghesani, V., Henry, M., Shwe, W., Lauricella, M., Miller, Z., Deleon, J., Miller, B. L., Dronkers, N., Brambati, S. M., Seeley, W. W., Mandelli, M. L., & Gorno-Tempini, M. L. (2020). Task-free functional language networks: Reproducibility and clinical application. The Journal of neuroscience: the official journal of the society for neuroscience, 40(6), 1311–1320. doi: 10.1523/JNEUROSCI.1485-19.2019. PMCID: PMC7002153.
- Fan, J. M., Gorno-Tempini, M. L., Dronkers, N. F., Miller, B. L., Berger, M. S., & Chang, E. F. (2020). Data-driven, visual framework for the characterization of aphasias across stroke, post-resective, and neurodegenerative disorders over time. Frontiers in neurology, 11, 616764. doi: 10.3389/fneur.2020.616764. PMCID: PMC7801263.
2021
- Ries, S. K., Schendel, K. L., Herron, T. J., Dronkers, N. F., Baldo, J. V., & Turken, A. U. (2021). Neural underpinnings of proactive interference in working memory: Evidence from patients with unilateral lesions. Frontiers in neurology, 12, 607273. doi:10.3389/fneur.2021.607273. PMCID: PMC7902939.
- Ivanova, M. V., Herron, T. J., Dronkers, N. F., & Baldo, J. V. (2021). An empirical comparison of univariate versus multivariate methods for the analysis of brain-behavior mapping. Human brain mapping, 42(4), 1070–1101. doi:10.1002/hbm.25278. PMCID: PMC7856656.
- Schendel, K., Herron, T. J., Curran, B., Dronkers, N. F., Ivanova, M., & Baldo, J. (2021). Case study: A selective tactile naming deficit for letters and numbers due to interhemispheric disconnection. NeuroImage. Clinical, 30, 102614. doi:10.1016/j.nicl.2021.102614. PMCID: PMC8022252.
- Lukic, S., Borghesani, V., Weis, E., Welch, A., Bogley, R., Neuhaus, J., Deleon, J., Miller, Z. A., Kramer, J. H., Miller, B. L., Dronkers, N. F., & Gorno-Tempini, M. L. (2021). Dissociating nouns and verbs in temporal and perisylvian networks: Evidence from neurodegenerative diseases. Cortex; a journal devoted to the study of the nervous system and behavior, 142, 47–61. doi:10.1016/j.cortex.2021.05.006. PMCID: PMC8556704.
- Ivanova, M. V., Zhong, A., Turken, A., Baldo, J. V., & Dronkers, N. F. (2021). Functional contributions of the arcuate fasciculus to language processing. Frontiers in human neuroscience, 15, 672665. doi:10.3389/fnhum.2021.672665. PMCID: PMC8267805.
- Llorens, A., Tzovara, A., Bellier, L., Bhaya-Grossman, I., Bidet-Caulet, A., Chang, W. K., Cross, Z. R., Dominguez-Faus, R., Flinker, A., Fonken, Y., Gorenstein, M. A., Holdgraf, C., Hoy, C. W., Ivanova, M. V., Jimenez, R. T., Jun, S., Kam, J., Kidd, C., Marcelle, E., Marciano, D., Martin, S., Myers, N.E., Ojala, K., Perry, A., Pinheiro-Chagas, P., Riès, S.K., Saez, I., Skelin, I., Slama, K., Staveland, B., Bassett, D.S., Buffalo, E. A., Fairhall, A. L., Kopell, N. J., Kray, L. J., Lin, J. J., Nobre, A. C., Riley, D., Solbakk, A-K., Wallis, J.D., Wang, X.-J., Yuval-Greenberg, S., Kastner, S., Knight, R. T. & Dronkers, N. F. (2021). Gender bias in academia: A lifetime problem that needs solutions. Neuron, 109(13), 2047–2074.doi: 10.1016/j.neuron.2021.06.002. PMCID: PMC8553227.
- Lwi, S. J., Herron, T. J., Curran, B. C., Ivanova, M. V., Schendel, K., Dronkers, N. F., & Baldo, J. V. (2021). Auditory comprehension deficits in post-stroke aphasia: Neurologic and demographic correlates of outcome and recovery. Frontiers in neurology, 12, 680248.
doi:10.3389/fneur.2021.680248. PMCID: PMC8397517. - Ivanova, M.V., Akinina, Yu.S., Soloukhina, O.A., Iskra, E.V., Buivolova, O.V., Charbazcz, A.V., Stupina, E.A., Khudyakova M.V., Akhutina, T.V., & Dragoy, O. (2021). The Russian aphasia test: The first comprehensive, quantitative, standardized, and computerized aphasia language battery in Russian. PLoS one, 16(11), e0258946. doi:10.1371/journal.pone.0258946. PMCID: PMC8601577.
- Kuptsova, S., Dragoy, O., & Ivanova M.V. (2021). Switching attention deficits in post-stroke individuals with different aphasia types. Aphasiology, 1-28. doi:10.1080/02687038.2021.2002804. PMCID in progress.
2022
- Zhong, A. J., Baldo, J. V., Dronkers, N. F., & Ivanova, M. V. (2022). The unique role of the frontal aslant tract in speech and language processing. NeuroImage: Clinical, 34, 103020. doi: 10.1016/j.nicl.2022.103020. PMCID: PMC9095886.
- Tee, B.L., Li-Ying, L.K-C., Chen, T.F., Yan, C.T.Y, Tsoh, J.M.Y., Chan, A.L-T., Wong,A., Lo,R.Y., Lu, C.L., Wang, P.N., Lee, Y.C., Yang, G.F-P, Battistella, G., Allen, I.E., Dronkers, N.F., Miller, B.L. & Gorno-Tempini, M.L. (2022). Dysgraphia phenotypes in native Chinese speakers with primary progressive aphasia. Neurology, 98(22), e2245-e2257.doi: 10.1212/WNL.0000000000200350. PMCID: PMC9162166.
- Ivanova, M. & Dronkers, N. (2022) Aphasia: How our language system can “break”. Frontiers for young minds. 10:626477. doi: 10.3389/frym.2022.626477. PMCID in progress.
- Zyryanov, A., Stupina, E., Gordeyeva, E., Buivolova, O., Novozhilova, E., Akinina, Y., Bronov, O., Gronskaya, N., Gunenko, G., Iskra, E., Ivanova, E., Kalinovskiy, A., Kliuev, E., Kopachev, D., Kremneva, E., Kryuchkova, O., Medyanik, I., Pedyash, N., Pozdniakova, V., Pronin, I., Rainich, K., Reutov, A., Samoukina, A., Shlyakhova, A., Sitnikov, A., Soloukhina, O., Yashin, K., Zelenkova, V., Zuev, A., Ivanova, M.V., & Dragoy, O. (2022). ‘Moderate global aphasia’: A generalized decline of language processing caused by glioma surgery but not stroke. Brain and language, 224, 105057.doi:10.1016/j.bandl.2021.105057. PMCID: PMC8743859.
- Ivanova, M.V., Pappas, I., Inglis, B., Herron T., Baldo J., Mohyee R., Kayser, A., D’Esposito, M., & Dronkers, N.F. Cerebral perfusion in post-stroke aphasia and its relation to residual language abilities. bioRxiv, doi: https://doi.org/10.1101/2022.07.01.498516.
Book chapters
- Baldo, J.V. & Dronkers, N.F. (2017). Lesion studies. In De Groot, A. M., & Hagoort, P. (Eds.). Research methods in psycholinguistics and the neurobiology of language: A practical guide. (pp. 309-328). John Wiley & Sons.
- Baldo, J.V., Ivanova, M.V., Herron, T.J., Wilson, S.M. & Dronkers, N.F. (2022). Voxel-based lesion symptom mapping. In Pustina, D. & Mirman, D. (Eds.). Lesion-to-symptom mapping: Principles and tools. (pp. 95-118). Neuromethods, vol 180, Springer, New York, NY. https://doi.org/10.1007/978-1-0716-2225-4_5
- Dronkers, N.F. & Ivanova, M.V. The neuroscience of language and aphasia. In Crosson, B., Brown, G.G., Haaland, K. & King, T. (Eds.), APA handbook of neuropsychology, in press.
Contact us
510-846-8905
dronkers@berkeley.edu
ivanova@berkeley.edu
